Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (31): 5036-5043.doi: 10.3969/j.issn.2095-4344.2014.31.020
Previous Articles Next Articles
Microsurgical discectomy versus microendoscopic discectomy for treatment of lumbar disc herniations: a meta-analysis
Liu Meng-jun1, Du Bin1, Wei Xin-wei1, Wang Shi-hai1, Lin Qing1, Wang Song1, Chen Zhi-xin2
- 1First Clinical Medical College of Lanzhou University, Lanzhou 730000, Gansu Province, China; 2First Department of Orthopedics, Gansu Provincial People’s Hospital, Lanzhou 730000, Gansu Province, China
-
Received:2014-06-29Online:2014-07-23Published:2014-07-23 -
Contact:Chen Zhi-xin, M.D., Chief physician, First Department of Orthopedics, Gansu Provincial People’s Hospital, Lanzhou 730000, Gansu Province, China -
About author:Liu Meng-jun, Studying for master’s degree, First Clinical Medical College of Lanzhou University, Lanzhou 730000, Gansu Province, China
CLC Number:
Cite this article
Liu Meng-jun, Du Bin, Wei Xin-wei, Wang Shi-hai, Lin Qing, Wang Song, Chen Zhi-xin. Microsurgical discectomy versus microendoscopic discectomy for treatment of lumbar disc herniations: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(31): 5036-5043.
share this article
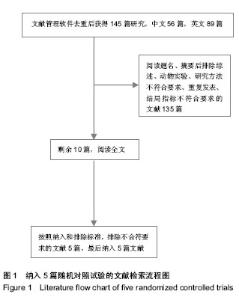
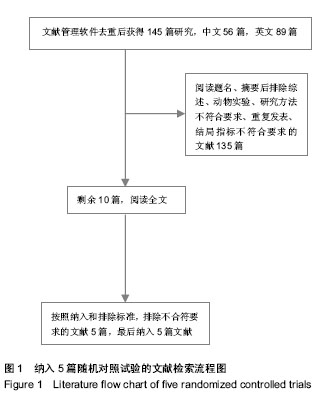
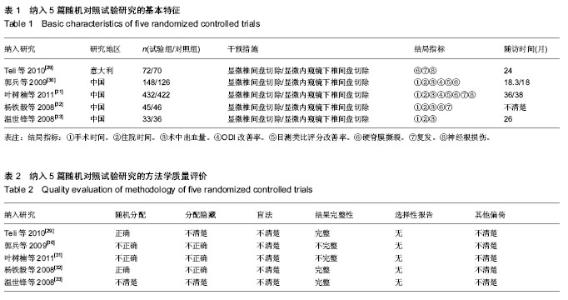
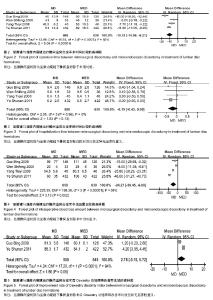
2.1 文献描述 文献管理软件去重后获得145篇相关对照研究,其中中文56篇,英文89篇,阅读题名、摘要后排除综述、动物实验、研究方法不符合要求、重复发表、结局指标不符合要求的文献135篇。对剩余10篇文献通过查看全文,排除了未达到纳入标准的5篇文献,最终纳入的5篇随机对照试验文献[29-33],共包括1 430例椎间盘突出患者(见图1),所有文献均对其基本情况进行比较,各组基线有一致性。纳入文献特征见表1。2.2 方法学质量评价 对所纳入文献按RevMan 5.2软件提供的质量评价标准进行偏倚风险评价:①随机方法是否正确。②是否采用分配隐藏。③是否采用盲法。④结果数据的完整性。⑤是否有选择性报告结果。⑥其他偏倚。结果见表2。"
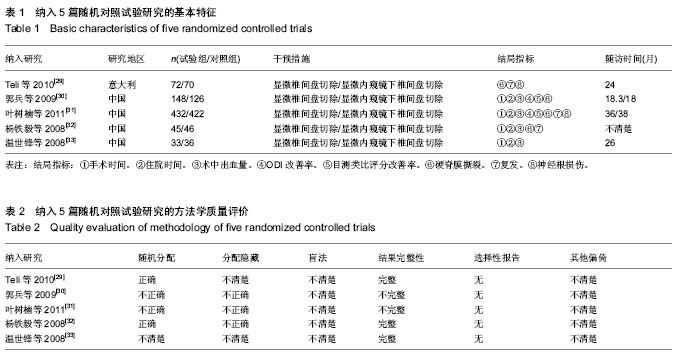
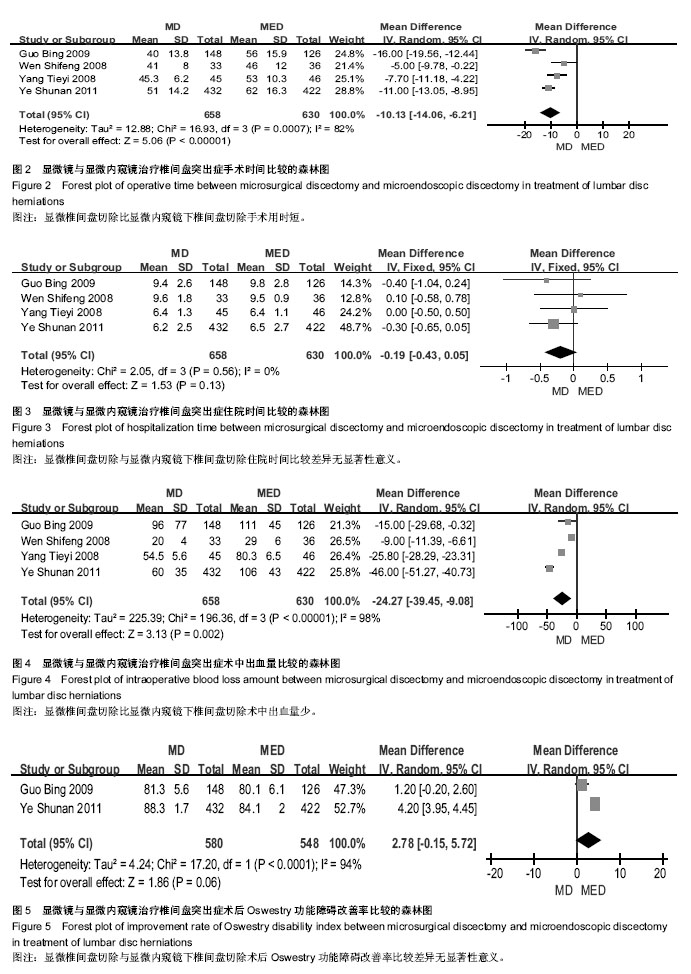
2.3 Meta分析结果 2.3.1 手术时间 4个研究比较了手术时间[30-33],各研究间存在统计学异质性(P=0.000 7,I2=82%),采用随机效应模型合并后进行Meta分析?结果显示两组差异有显著性意义[MD= -10.13(-14.06,-6.21),P < 0.000 01],说明显微椎间盘切除比显微内窥镜下椎间盘切除手术用时短(图2)? 2.3.2 住院时间 4个研究比较了住院时间[30-33],各研究间无统计学异质性(P=0.56,I2=0%),采用固定效应模型合并后进行Meta分析?结果显示两组差异无显著性意义[MD= -0.19(-0.43,0.05),P=0.13],说明显微椎间盘切除与显微内窥镜下椎间盘切除住院时间相当(图3)? 2.3.3 术中出血量 4个研究比较了术中出血量[30-33],各研究间存在统计学异质性(P < 0.000 01,I2=98%),采用随机效应模型合并后进行Meta分析?结果显示两组差异有显著性意义[MD=-24.27(-39.45,-9.08),P=0.002],说明显微椎间盘切除比显微内窥镜下椎间盘切除术中出血量少(图4)? 2.3.4 ODI改善率 2个研究比较了两组ODI改善率[30-31],各研究间存在统计学异质性(P < 0.000 1,I2=94%),采用随机效应模型合并后进行Meta分析?结果显示两组差异无显著性意义[MD=2.78 (-0.15,5.72),P=0.06],说明显微椎间盘切除与显微内窥镜下椎间盘切除在ODI改善率方面相当(图5)?"
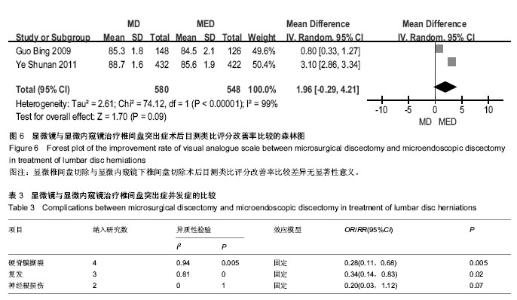
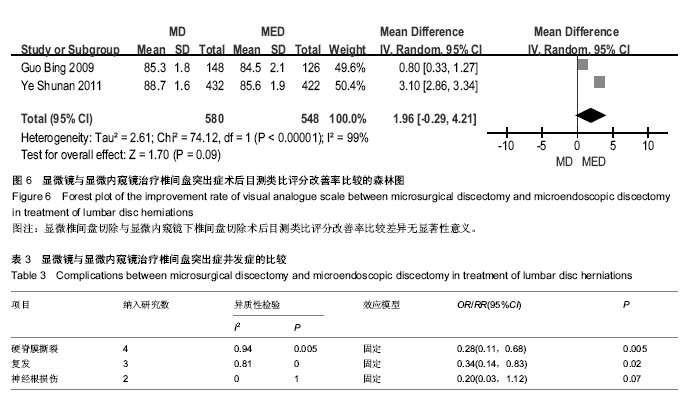
2.3.5 目测类比评分改善率 2个研究比较了目测类比评分改善率[30-31],各研究间存在统计学异质性(P < 0.000 01, I,采用随机效应模型合并后进行Meta分析?结果显示两组差异无显著性意义[MD=1.96(-0.29,4.21), P,说明显微椎间盘切除与显微内窥镜下椎间盘切除在目测类比评分改善率方面相当(图6)?=0.09]2=99%) 2.3.6 硬脊膜撕裂 4研究比较了硬脊膜撕裂[29-32],各研究间无统计学异质性(P=0.94,I2=0%),采用固定效应模型合并后进行Meta分析?结果显示两组差异有显著性意义[RR=0.28(0.11,0.68),P=0.005],说明显微椎间盘切除比显微内窥镜下椎间盘切除硬脊膜撕裂发生率低(表3)? 2.3.7 复发 3个研究比较了复发[29, 31-32],各研究结果间无统计学异质性(P=0.81,I2=0%),采用固定效应模型合并后进行Meta分析?结果显示两组差异无显著性意义[RR= 0.34(0.14,0.83),P=0.02],说明显微椎间盘切除比显微内窥镜下椎间盘切除复发率低(表3)? 2.3.8 神经根损伤 2个研究比较了神经根损伤[29, 31],各研究结果间无统计学异质性(P=1.00,I2=0%),采用固定效应模型合并后进行Meta分析?结果显示两组差异无显著性意义[RR=0.20(0.03,1.12),P=0.07],说明两种微创方式在神经根损伤方面相当(表3)。"
| [1] Gibson JN, Waddell G.Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine (Phila Pa 1976). 2007; 32(16):1735-1747. [2] Andrews DW, Lavyne MH. Retrospective analysis of microsurgical and standard lumbar discectomy. Spine (Phila Pa 1976). 1990; 15(4):329-335. [3] Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong). 2011;19(1):30-34. [4] Righesso O, Falavigna A, Avanzi O, et al. Correlation Between Persistent Neurological Impairment and Clinical Outcome After Microdiscectomy for Treatment of Lumbar Disc Herniation. Neurosurgery. 2012; 70(2): 390-396. [5] Merk H, Krämer R, Baltzer AW, et al. Microsurgical lumbar intervertebral disk operation. Technique and complications. Orthopade. 1999; 28(7):593-597. [6] Katayama Y, Matsuyama Y, Yoshihara H , et al. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech. 2006; 19(5):344-347. [7] Soliman J, Harvey A, Howes G, et al. Limited microdiscectomy for lumbar disk herniation: a retrospective long-term outcome analysis. J Spinal Disord Tech. 2014; 27(1):E8-E13. [8] Kambin P, Savitz MH. Arthroscopic microdiscectomy: an alternative to open disc surgery. Mt Sinai J Med. 2000; 67(4): 283-287. [9] Nakagawa H, Kamimura M, Uchiyama S, et al. Microendoscopic discectomy (MED) for lumbar disc prolapse. J Clin Neurosci. 2003; 10(2):231-235. [10] Yadav YR, Parihar V, Namdev H, et al. Endoscopic Interlaminar Management of Lumbar Disc Disease. J Neurol Surg A Cent Eur Neurosurg. 2013; 74(2): 77-81. [11] Wu X, Zhuang S, Mao Z, et al. Microendoscopic discectomy for lumbar disc herniation - Surgical technique and outcome in 873 consecutive cases. Spine. 2006; 31(23): 2689-2694. [12] Katayama Y, Matsuyama Y, Yoshihara H, et al. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: A prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech. 2006;19(5): 344-347. [13] Nakagawa H, Saito K, Mitsugi T, et al. Microdiscectomy and foraminotomy in cervical spondylotic myelopathy and radiculopathy:anterior versus posterior, microendoscopic surgery versus mini-open microsurgery. World Neurosurg. 2014; 81(2): 292-293. [14] Oztürk C, Tezer M, Aydogan M, et al. Posterior endoscopic discectomy for the treatment of lumbar disc herniation. Acta Orthop Belg. 2006; 72(3):347-352. [15] Kaliaperumal C, Kuechler D, Kaar G, et al. Does surgical technique affect the incidence of spondylodiscitis post-lumbar microdiscectomy? A retrospective analysis of 3063 patients. Spine (Phila Pa 1976). 2013; 38(4):364-367. [16] Kulkarni AG, Bassi A, Dhruv A. Microendoscopic lumbar discectomy: Technique and results of 188 cases. Indian J Orthop. 2014; 48(1):81-87. [17] Türeyen K.One-level one-sided lumbar disc surgery with and without microscopic assistance: 1-year outcome in 114 consecutive patients. J Neurosurg. 2003; 99(3 Suppl): 247-50. [18] Byval'tsev VA, Sorokovikov VA, Egorov AV, et al. Comparative analysis of effectiveness of endoscopic, microsurgical and endoscopic-assisted diskectomy in treatment of patients with lumbar intervertebral disk herniations. Zh Vopr Neirokhir Im N N Burdenko. 2010; (4):20-26. [19] Hussein M, Abdeldayem A, Mattar MM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J. 2014. [20] Wang M, Zhou Y, Wang J, et al. A 10-year follow-up study on long-term clinical outcomes of lumbarmicroendoscopic discectomy. J Neurol Surg A Cent Eur Neurosurg. 2012; 73(4):195-198. [21] Casal-MoroR, Castro-Menéndez M, Hernández-Blanco M, et al. Long-term outcome after microendoscopic diskectomy for lumbar disk herniation: a prospective clinical study with a 5-year follow-up. Neurosurgery. 2011; 68(6):1568-1575. [22] Zhou Y, Wang M, Wang J, et al. Clinical experience and results of lumbar microendoscopic discectomy: a study with a five-year follow-up. Orthop Surg. 2009; 1(3):171-175. [23] Husain M, Jha DK, Agrawal S, et al. Conical working tube: a special device for endoscopic surgery of herniated lumbardiscs. J Neurosurg Spine. 2005; 2(3):265-270. [24] Riesenburger RI, David CA. Lumbar microdiscectomy and microendoscopic discectomy. Minim Invasive Ther Allied Technol. 2006; 15(5): 267-270. [25] Schizas C, Tsiridis E, Saksena J. Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery. 2005;57(4):357-360. [26] Smith JS, Ogden AT, Shafizadeh S, et al. Clinical Outcomes After Microendoscopic Discectomy for Recurrent Lumbar Disc Herniation. J Spinal Disord Tech. 2010; 23(1):30-34. [27] Arts MP, Brand R, van den Akker ME, et al. Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA. 2009; 302(2):149-158. [28] Arts MP,Brand R, van den Akker ME, Koes BW, et al. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Minim Invasive Ther Allied Technol. 2006; 15(5):267-270. [29] Teli M, Lovi A, Brayda-Bruno M, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010; 19(3): 443-450. [30] 郭兵,邵增务,熊蠡茗,等.显微镜与显微内窥镜下微创手术治疗腰椎间盘突出症的疗效比较[J].中国脊柱脊髓杂志, 2009, 19(5): 360-364. [31] 叶树楠,杨述华,邵增务,等.手术显微镜下与椎间盘镜下治疗腰椎间盘突出症的比较研究[J].中华骨科杂志, 2011, 31(10): 1138-1143. [32] 杨铁毅,刘树义,刘粤,等.内窥镜下椎间盘切除术与显微椎间盘摘除术的比较研究[J].脊柱外科杂志, 2008, 6(4): 217-220. [33] 温世锋,刘恩志,郭东明,等.显微镜与椎间盘镜辅助腰椎间盘切除术治疗腰椎间盘突出症疗效的对比分析[J].中华显微外科杂志, 2008, 31(2): 104-106. [34] 苗洁,仝超,赵洪波,等.腰椎间盘突出症两种微创手术方法比较[J]. 中国骨与关节损伤杂志, 2006, 21(12): 991-992. [35] 刘庆国,宋志斌,高建伟,等.腰椎间盘镜手术和显微手术治疗腰椎间盘突出症的系统评价[J].中国现代神经疾病杂志, 2012,12(4): 399-406. [36] Smith N, Masters J, Jensen C, et al. Systematic review of microendoscopic discectomy for lumbar disc herniation. Eur Spine J. 2013; 22(11):2458-2465. [37] Ali A, Baraliakos X, Kanawati B, et al. Microsurgical nerve root decompression in scoliotic lumbar spines-the relationship between important anatomical structures in correlation to imaging and implications for daily practice: anatomic cadaveric study. J Neurosurg Spine. 2010; 13(1):123-132. [38] Martin-Laez R, Martinez-Agueros JA, Suarez-Fernandez D, et al. Complications of endoscopic microdiscectomy using the EASYGO! system: is there any difference with conventional discectomy during the learning-curve period? Acta Neurochir (Wien). 2012; 154(6): 1023-1032. [39] Aljabi Y, El-Shawarby A, Cawley DT, et al. Effect of epidural methylprednisolone on post-operative pain and length of hospital stay in patients undergoinglumbar microdiscectomy. Surgeon. 2014. [Epub ahead of print] [40] Kambin P, Cohen LF, Brooks M, et al.Development of degenerative spondylosis of the lumbar spine after partial discectomy. Comparison of laminotomy, discectomy, and posterolateral discectomy. Spine (Phila Pa 1976). 1995; 20(5):599-607. [41] Findlay GF, Hall BI, Musa BS, et al. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine (Phila Pa 1976). 1998;23(10):1168-1171. [42] Schick U, Döhnert J, Richter A, et al. Microendoscopic lumbar discectomy versus open surgery: an intraoperative EMG study. Eur Spine J. 2002; 11(1):20-26. [43] Hermantin FU, Peters T, Quartararo L, et al. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999; 81(7):958-965. [44] Ranjan A, Lath R. Microendoscopic discectomy for prolapsed lumbar intervertebral disc. Neurol India. 2006; 54(2):190-194. [45] Arts MP, Brand R, van den Akker ME, et al. Results and risk factors for recurrence following single-level tubular lumbar microdiscectomy. J Neurosurg Spine. 2010; 12(6):680-686. [46] Matsumoto M, Watanabe K, Hosogane N, et al. Incidence of complications associated with spinal endoscopic surgery: nationwide survey in 2007 by the Committee on Spinal Endoscopic Surgical Skill Qualification of Japanese Orthopaedic Association. J Orthop Sci. 2010; 15(1): 92-96. [47] Shin DA, Kim KN, Shin HC, et al. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008; 8(1):39-43. [48] Nowitzke AM. Assessment of the learning curve for lumbar microendoscopic discectomy. Neurosurgery. 2005; 56(4): 755-762. [49] Arts MP, Peul WC, Brand R, et al. Cost-effectiveness of microendoscopic discectomy versus conventional open discectomy in the treatment of lumbar disc herniation: a prospective randomised controlled trial. BMC Musculoskelet Disord. 2006; 7:42. |
| [1] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [2] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [3] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [4] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [5] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [6] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [7] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [8] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [9] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [10] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [11] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [12] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| [13] | Li Yang, Zhang Mingyong. Meta-analysis of the effect of double Endobutton and clavicular hook plate on the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 463-470. |
| [14] | Li Yanle, Yue Xiaohua, Wang Pei, Nie Weizhi, Zhang Junwei, Tan Yonghai, Jiang Hongjiang. Intramedullary nail fixation versus plate fixation in the treatment of displaced midshaft clavicular fractures in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 471-476. |
| [15] | Liu Chang, Han Shufeng. Interlocking intramedullary nail for proximal femur versus proximal femoral anti-rotation intramedullary nail or proximal femoral anti-rotation intramedullary nail of Asian for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 477-485. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||